Your DNA determines an overwhelming amount of information about who you are, what you look like, and how certain environmental factors influence your overall health. This is why at the Institute for Human Optimization, we aim to be a wellness intelligence partner for our patients, using the latest genomic testing to empower them to reach their full human potential. By generating your unique comprehensive genomic profile, we are able to gain insight into your genetic makeup and help you take your health into your own hands. In this week’s post, we’re discussing the human genome, and how we help our patients use this knowledge for the prevention, early diagnosis, and personalized treatment of complex, chronic conditions.
In virtually every cell of your body is a complete copy of the three billion DNA base pairs that make up the human genome.
The study of the human genome is different from the study of genetics in that it focuses on the entirety of the genetic makeup and tries to sequence it. This is an ongoing research subject, mainly carried out by the Human Genome Project. But why is this important to you and your personal health journey?
Everything starts in the genome- from what you look like, to what disorders you’re predisposed to, to what foods you should and shouldn’t eat, it’s all there. And thanks to decades of research, we now have advanced molecular testing that can predict how genes are behaving by assessing their structural makeup and biochemical expressions.
At the Institute for Human Optimization, we utilize what we refer to as a “genotype to phenotype approach”. Your phenotype is the physical expression of the genome. It’s the way your genome produces blue eyes instead of brown, or curly hair instead of straight. It’s the way your genes influence your resting heart rate, blood pressure, or response to stress. These traits can be measured and therefore, manipulated.
An article in the New England Journal of Medicine describes how our genes are marked by experience. There are molecular “tags” that influence gene expression, even to the effect of “turning up or down the volume” on specific genes. For example,
“Men whose grandfathers were exposed to the Swedish famine in Överkalix before puberty tend to die at an earlier age from various common diseases than men whose grandfathers were not exposed to the famine. Both the Dutch Hunger Winter and the Great Leap Forward of China involved mass starvation of the population, and in both cases, fetal exposure to famine during the first trimester of gestation was associated with an incidence of schizophrenia in adulthood that was twice as high as the incidence among adults who had not been exposed during gestation.”
N Engl J Med 2018; “The Key Role of Epigenetics in Human Disease Prevention and Mitigation”
DOI: 10.1056/NEJMra1402513
By combining individualized genomic blueprint analysis and phenotypic biomarkers as well as biometric data tracking over time, the Institute is able to help us guide your health decisions, behavioral patterns, and therapeutic interventions. In return, there’s the potential for improved health outcomes, quality of life, and longevity.
Your life choices affect how your genes are expressed, and the only way to find out how to hack this system is with genome testing.
How We Test
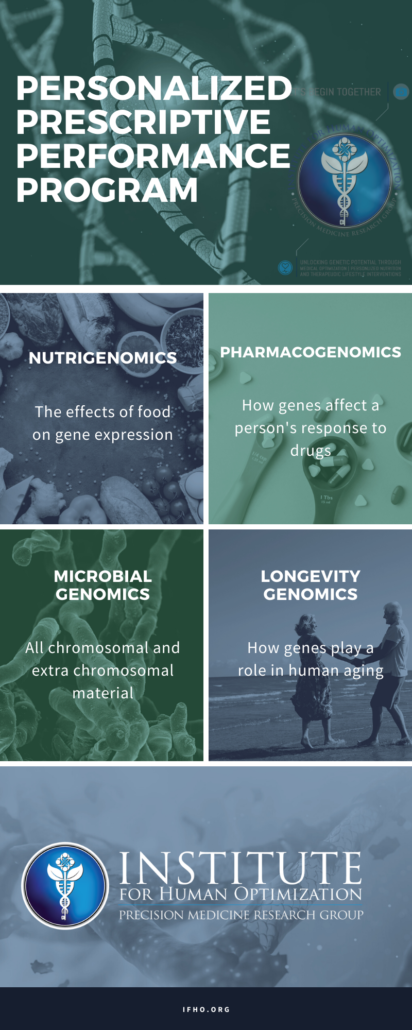
As an institution that prioritizes hard data over trial and error, we use advanced molecular testing to map out your personal genome and apply this data into what we call a “Personalized Prescriptive Performance Program“. Your genetic makeup, lifestyle, and goals are not the same as the next person’s, so why should your healthcare strategy mirror theirs?
To get the basis for your program, we rely on the cutting edge software developed by Dr. Peter D’ Adamo, Opus23. It uses a sample of your DNA to generate a report detailing any genetic discrepancies you may have. There are distinct polymorphisms that can occur within the genes that change the way those genes are expressed. We covered this in a previous blog post, “Epigenetics: How to Control Your Gene Expression”.
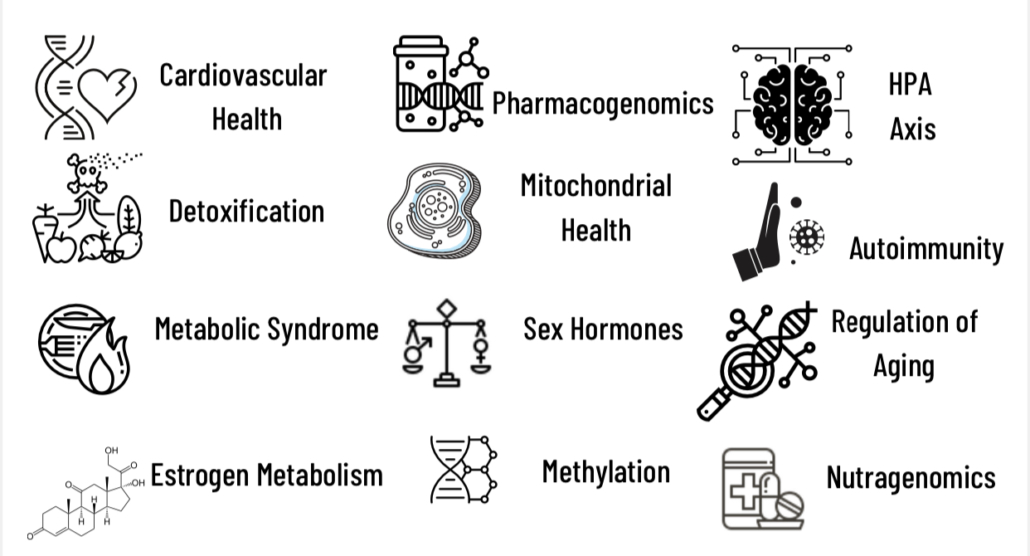
Genomic testing is used to evaluate common genetic variations known as single nucleotide polymorphisms (SNPs). The presence of specific SNPs may indicate a predisposition for health vulnerabilities. SNPs may be assessed in multiple functional areas including cardiovascular, detoxification, methylation, immune modulation, and estrogen metabolism.
By understanding your genetic foundation, we can recommend vitamins, supplements, and therapies to truly optimize your health. This information can give you insight into how your genes are behaving and how to tackle possible health problems at their root cause before they begin. Prevention is always better than a cure.
The platform we use reports on over 5,200 SNP variants and their influence on:
The Future of Healthcare
The Institute for Human Optimization operates on the principles of integrative and functional medicine. We believe the future of healthcare lies in educating patients on how to live their lives in a way that promotes health and builds up resiliency so old age is not synonymous with disease and chronic illness.

Using a variety of testing methods as well as a detailed client intake process, we create a Personalized Prescriptive Performance Program for your unique genome and goals using the following:
- Nutrigenomics – the way your genes dictate how your body metabolizes vitamins, minerals, and nutrients. For example, a polymorphism in the BCO1 gene can cause a person to not metabolize vitamin A correctly. Supplementing with extra vitamin A may be helpful in negating health consequences from having this genetic polymorphism.
- Pharmacogenomics – Offers insight into predicting drug responses and clinical outcomes. It can be used to reduce adverse events, and select the correct dosing and timing of administration of medications. This is largely due to the metabolizer status of the individual.
- Microbial Genomics – the way our genes influence our resident microbiome population and biodiversity. For example, FUT2 gene variations influence an individual’s sector potential of placing an H antigen oligosaccharide on the intestinal mucosa which acts as both an attachment site and a carbon source for intestinal bacteria.
- Longevity Genomics – the study of longevity genes is a developing science. It is estimated that about 25 percent of the variation in the human life span is determined by genetics, but which genes, and how they contribute to longevity, are not well understood. A few of the common variations (called polymorphisms) associated with long life spans are found in the APOE, FOXO3, and CETP genes, but they are not found in all individuals with exceptional longevity.
By detailing your genome, we can often predict what will happen before it does. We can understand how your body is functioning and what we need to do to optimize your health from the genome to the phenome.
To schedule a consultation with the Institute for Human Optimization or find out more about genome testing and the Opus23 software, click here.