The gut-brain axis is a term that refers to the two-way communication system between the gastrointestinal tract and the central nervous system. The gut-brain axis can be disrupted by many different factors, including stress. With an unhealthy gut microbiome (bacteria) in your digestive tract, you are more susceptible to many health conditions. These include inflammation, metabolic syndrome, obesity, type 2 diabetes, depression or anxiety disorders, and neurodegenerative diseases such as Alzheimer’s disease or Parkinson’s disease.
The purpose of this blog post is to share information on how a healthy diet can help heal your gut microbiome by providing proper nourishment for good bacteria while helping remove bad bacteria from your body through natural detoxification pathways.
. . .
WHAT IS THE GUT-BRAIN AXIS?
The Gut-Brain Axis has recently been coined as the new “Central Nervous System”, which is a complex system of communication between the enteric nervous system in the gut and the central nervous system (CNS) in your brain. The Gut-Brain Axis is responsible for maintaining homeostasis between the autonomic nervous system and the immune system, regulating substances that may act as neurotransmitters. When the Gut-Brain Axis is not functioning optimally, this can lead to a range of problems including depression, anxiety, and stress-related disorders. Gut bacteria are responsible for maintaining the Gut-Brain Axis by producing neurotransmitters that can stimulate specific cells in the gut which can then send signals back to the brain through various neurological pathways.
Strong evidence suggests that gut microbiota has an important role in bidirectional interactions between the gut and the nervous system. It interacts with CNS by regulating brain chemistry and influencing neuro-endocrine systems associated with stress response, anxiety, and memory function. Gut microbiota can also influence brain function through the hypothalamic-pituitary-adrenal axis and autonomic nervous system. The hypothalamic-pituitary-adrenal axis is the major neuroendocrine system that mediates the stress response. Our autonomic nervous system is made up of the sympathetic nervous system (SNS) which is activated by stress and can stimulate colonic relaxation, vasoconstriction, and ileocaecal transit. Gut microbiota also interacts with immune cells in the gut, and these interactions have been shown to affect brain function. This has implications for mood disorders such as anxiety and depression that we will discuss later in this blog. Gut microbiota can also influence brain function through the autonomic nervous system, which regulates all of our unconscious actions (our heart rate, breathing pattern, etc).
Another factor worth mentioning is neurotransmitters. Neurotransmitters are essentially electrical signals in the brain that help us communicate and regulate many bodily functions including mood, emotions, ability to handle stress, and more. When our gut-health axis is off, our neurotransmitter signals can be disrupted which causes a cascade of brain issues. To make this simple, we are going to focus on serotonin as an example of what our gut-health axis can do for us. Serotonin is a neurotransmitter that regulates mood and behavior. When serotonin levels get messed up, it not only causes anxiety but also disrupts sleep patterns and more.
GUT HEALTH AND MENTAL HEALTH
Gut health is essential to mental health because it affects our mood, emotions, ability to handle stress, and symptoms of conditions such as Autism Spectrum Disorder (ASD). The Gut-Brain Axis is a two-way street, and both of these ‘roads’ are connected. When one road is in bad condition it affects the other road as well. This can cause inflammation, stress, and disease. As we learned in our inflammation series, inflammation can cause an increase in the release of cortisol from the adrenal glands. This is not good for us because too much cortisol disrupts our body and brain functions.
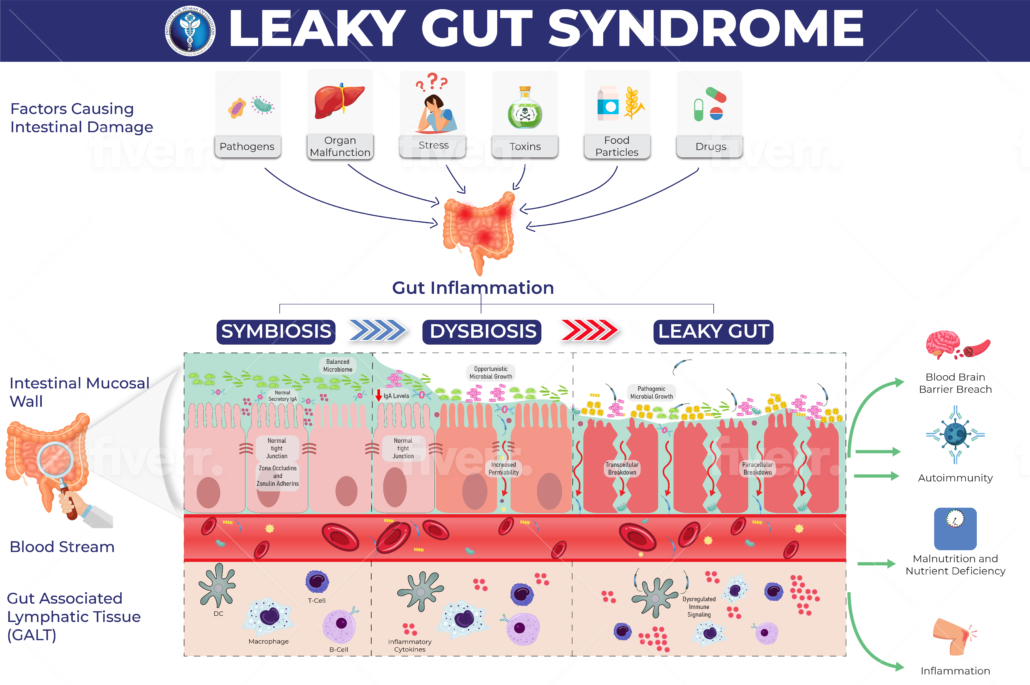
Stress also plays a large role in our gut-brain axis. Not only does stress cause our adrenal glands to release cortisol, but it can also lead to poor diet decisions that throw off your gut bacteria. Anxiety and depression are associated with changes in microbiome composition, as well as with increased gut permeability allowing lipopolysaccharides. (LPS) refers to metabolic endotoxemia. LPS are not only harmful to your gut, but they are also a primary cell wall component of gram-negative bacteria. So as stress and anxiety increase your gut permeability and release lipopolysaccharides into the bloodstream these can cause inflammation in the brain leading to more cortisol production and an overall increase in inflammation throughout the body.
IMPORTANCE OF OPTIMAL GUT HEALTH
Maintaining good gut health is important as the gut microbiome may help with stress responses by influencing the synthesis of neurotransmitters and neuropeptides that have an impact on homeostasis, neuroinflammation, and neuronal plasticity. Recent research shows that the gut microbiome may also have an impact on neurogenesis. Neurogenesis is a vital process to maintaining mental health and is the generation of neurons from neural stem cells. Gut microbiota close to the enteric nervous system (ENS) exerts substantial influence over it. The gut microbiome can stimulate vagal afferent neurons by releasing transmitters such as 5-HT, acetylcholine, and norepinephrine. The gut microbiome can also stimulate afferent neurons in the submucosal and myenteric plexus of the ENS to release a range of chemicals including neuropeptides (e.g., substance P, cholecystokinin)
HOW IS THE GUT-BRAIN AXIS BEING USED IN MEDICINE TODAY?
Research is still underway on how to improve the balance of gut microbiota or modulate the gut-brain axis. Gut microbiome therapy may be used in some future medical therapies for psychiatric disorders, autism, and neurodegenerative disease.
Biological psychiatry is currently studying the Gut-Brain Axis by focusing on how metabolites from the microbiome can impact neurotransmitter function, synaptic plasticity, and neuroinflammation. The Gut-brain axis is being studied in clinical psychiatry for treating conditions like depression, anxiety disorders, and autism spectrum disorder (ASD). Although research is still underway on how to improve the balance of gut microbiota or modulate the gut-brain axis, some recent studies have been completed for Gut microbiome therapy.
WHAT CAN YOU DO AT HOME TO IMPROVE OUR GUT-BRAIN AXIS
Diet is one of the most important modifying factors of the microbiota-gut-brain axis. If you are experiencing any gastrointestinal symptoms (gas, bloating, stomach pain) as well as mental health issues such as anxiety or depression then a Gut-Brain Axis evaluation is recommended to determine if there is an imbalance in neurotransmitters due to the Gut-Brain Axis not functioning efficiently. The most important thing that you can do if you’re not feeling like yourself is to visit your Provider and get these tests done!
In the meantime, it is important to improve your Gut-Brain Axis by trying the following tips to get back on track:
- Get enough fiber in your diet from fruits and vegetables
- Get rid of the bad bacteria’s and yeast with beneficial bacteria
- Reduce stress as much as possible and practice self-care!
- Exercise regularly
- Practice mindfulness
The Gut-Brain Axis is the intersection of your gut and brain that affect each other. When your Gut-Brain Axis isn’t set up correctly it can be harmful to your overall well-being. This new discovery has been coined as the “central nerve” for all three major organ systems–the CNS, endocrine, and immune systems. It’s not just about digestion anymore! If you want to learn more about how this process works or if you’re looking to improve health with an integrative approach to optimal gut health – check out our most recent blogs. Follow us next week as we take on: Metabolic Endotoxemia.
At the Institute for Human Optimization, we understand that what starts in the gut impacts the entire body. No two patients are the same, so we work with you and create a personalized and individual approach to your gut health issues. What can that look like? Would you plant grass seed or kill the weeds first? Weeds should be killed first. Similarly, we will work directly with you to reduce or remove the weeds, aka factors that are driving dysbiosis. After that, we can work together to restore balance in your gut microbiome.
Disclaimer: The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Additionally, the information provided in this blog, including but not limited to, text, graphics, images, and other material contained on this website, or in any linked materials, including but not limited to, text, graphics, images are not intended and should not be construed as medical advice and are for informational purposes only and should not be construed as medical advice. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this or any website.